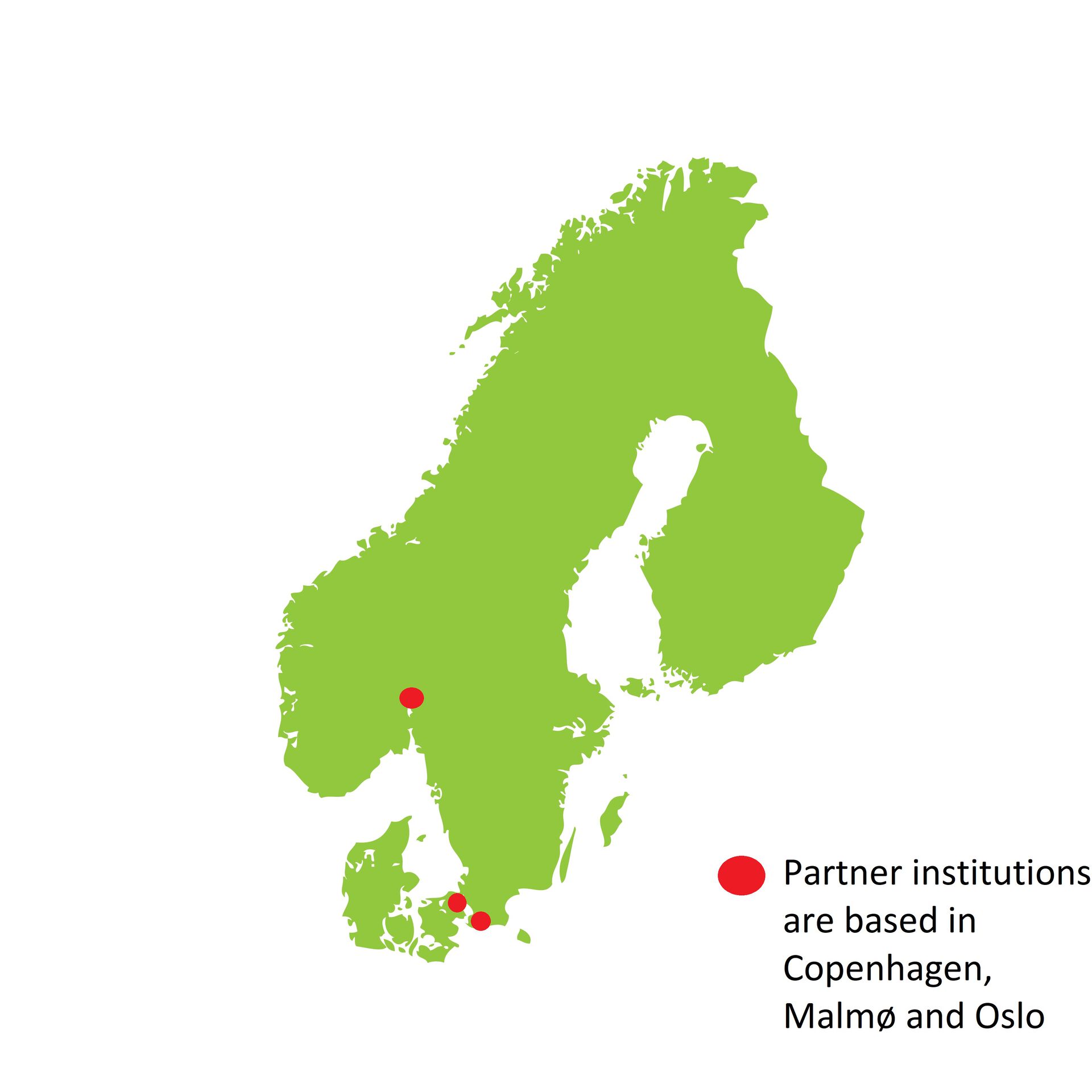
The project is part of the Born in the twilight program, funded by the Olav Thon Foundation, with partners in Norway, Denmark and Sweden.

Aims
We aim to
- gain insight into how the microbiome and the collection of resistance genes carried by the microbiome, the resistome, develop in preterm infants in response to different antibiotic interventions.
- identify if disadvantageous developments of the microbiome can be prevented by supportive treatment with the recently described HAMLET-protein
The results are expected to
- provide increased knowledge on human microbiome and resistance development,
- develop new strategies to fight antibiotic resistance, and
- provide information to better guide antibiotic use in preterm infants
Progress
The group held its kick-off meeting at the University of Oslo on the 12th March, 2018, with representatives from Sweden and Denmark.
We have gained all the necessary approvals and collection of samples has started. In this longitudinal study, samples will be collected from preterm babies born in the period between 2019 and early 2021.
- We are working on the establishment of a model that aims to reproduce the microbiome of the respiratory tract of preterm babies in the laboratory.
This model will enable using the samples from the babies to test antibiotics alone or in combination with antimicrobials found in breast milk, for their effects on the microbiome.
- The group has established the methodology to perform functional metagenomics.
Together with shotgun metagenomics, this method will enable the idenficiation of new and functional antibiotic restistance genes in the preterm babies.
Animal models
We are using neonatal mouse models to study the impact of clinically relevant antibiotic regimens on the infant microbiota and immune system. Specifically, we investigate:
- how antibiotics alter the composition and diversity of the microbiota; and
- how antibiotics modulate the innate and adaptive immune responses.
An Analytical Tool
![]()
We are also working on the design of a analytical and visualization tool, the ResistoXlorer, that will be used in the project for characterization of the microbiome and the resistomes. ResistoXplorer is also intended to benefit the entire scientific community by launching it as an online tool that can be accessed by all, both clinicians and researchers and other interested parties, for better surveillance, monitoring and decision making for antibiotic usage and understanding of resistome development.
Research Group
The research group is represented by a distinctive combination of expertise in pediatric neonatology, infectious diseases, public health, molecular biology and microbiology:
.png)
Bottom left: Anna Torwick, Rabia Khan, Fernanda Petersen, Gabriela Salvadori da Silva, Heidi Aarø Åmdal.
Project Leader
Professor Fernanda Petersen, Department of Oral biology, UiO
Partners in Denmark
Dr. Ulrik Lausten-Thomsen, Department of Neonatology at the Juliane Centre, Rigshospitalet, Copenhagen University Hospital, Denmark
Professor Gorm Greisen, professor of Paediatrics at the Department of Neonatology at the Juliane Centre, Rigshospitalet, Copenhagen University Hospital and the University of Copenhagen
Partner in Sweden
Professor Anders Hakansson, Professor at Experimental Infection Medicine, Lund University, Malmö, Sweden
Partners in Norway
Dr Kirsti Haaland, Neonatology, Oslo University Hospital
Prof. Dag Berild, Department of Infectious Diseases, Oslo University Hospital, and University of Oslo
Prof. Ola Didrik Saugstad, Professor emeritus at Paediatric Research UiO and Oslo University Hospital
Ulf Dahle, Specialist Director, Infection Control and Environmental Health, Norwegian Institute of Public Health
Professor Thomas Kuntziger, Department of Oral biology, UiO
Researcher
Sudhanshu Shekhar, Department of Oral biology, UiO
Postdoctorate Fellows
Roger Junges, Department of Oral biology, UiO
Gabriela Salvadori Silva, Department of Oral biology, UiO
PhD Candidates
Achal Dhariwal, Department of Oral Biology, UiO,
Polona Rajar, Department of Oral biology, UiO and OUS
Navdeep Kaur Brar, Department of Oral Biology, UiO
Head Engineer
Heidi Aarø Åmdal, Department of Oral Biology, UiO
Administration and coordination
Anna Torwick, Department of Oral Biology, UiO
.png?1593003573326)
Funding


Additional Funding

